Gastric Sleeve Recovery Guide
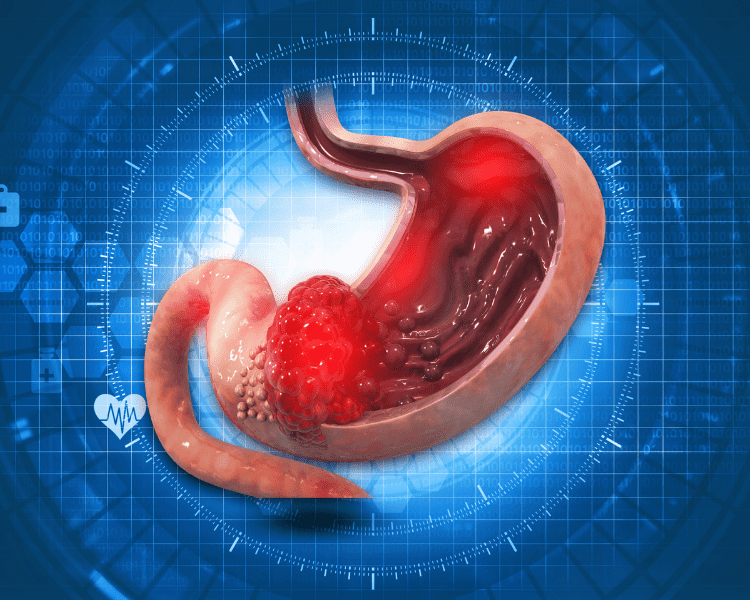
The gastric sleeve surgery, or sleeve gastrectomy, is a popular bariatric surgery that helps individuals achieve significant weight loss and improve their overall health. Surgical intervention for obesity is a transformative procedure that can have a profound and lasting effect. However, It requires careful planning and preparation before the surgery, as well as knowledge and dedication to follow through during recovery. In this blog, we will provide a comprehensive recovery guide for individuals undergoing gastric sleeve surgery.

Gastric Sleeve Recovery Timeline
- 24 to 48 Hours Post-Op: Patients may experience mild discomfort or pain near the surgical area. You’ll be on a clear liquid diet and may start walking under medical supervision. You are not allowed to eat first 6 hours after gastric sleeve and smoking is not allowed for up to 3 months after surgery.
- 3 Days to 1 Week Post-Op: Transition to a full liquid diet, including protein shakes and soup broth. Light physical activity is encouraged. You should be able to start regular activity, such as walking or light jogging, but avoid intense exercise until 4 weeks post-op.
- 2 Weeks Post-Op: Begin a pureed diet. Continue with light physical activities.
- 3 Weeks to 1 Month Post-Op: Gradually shift to a soft food diet. Begin moderate physical activities.
- 1 Month to 3 Months Post-Op: Transition to a long-term diet plan with a focus on high-protein, low-sugar, and low-fat foods. Continue moderate physical activity, gradually increasing its intensity.
- 3 Months Onwards: By now, you should be fully adjusted to your new dietary habits and regular physical activity. Regular follow-ups with your bariatric team are crucial to monitor your progress and make necessary adjustments.
What to Expect After Gastric Sleeve Surgery
Undergoing gastric sleeve surgery is a major step towards improving your health and quality of life. However, understanding what happens after the procedure is just as important as the surgery itself. From hospital care to emotional changes, knowing what to expect can ease worries and help you prepare for this new chapter in your journey. Below, we’ll cover essential points to help you navigate the immediate aftermath.
The First 24 Hours
Right after surgery, you’ll wake up in the recovery room, still under medical supervision. During this time, healthcare staff will closely monitor your vital signs, including heart rate, blood pressure, and oxygen levels, ensuring everything remains stable. You’ll likely feel groggy from the anaesthesia, which is perfectly normal.
Pain management is a top priority during the first day. Your medical team will administer pain relief to keep discomfort under control. Most patients describe the pain as manageable, often feeling more like soreness or tightness in the abdomen rather than sharp pain. If the discomfort feels intense, let your care team know—they’re there to keep you comfortable.
You might also notice devices such as IV drips for hydration and medication or compression sleeves on your legs to prevent blood clots. Although it may seem overwhelming, these are standard precautions to promote recovery.
Additionally, surgeons will want you to start moving as soon as possible, even if it’s just sitting up or standing with help. Light movement reduces the risk of complications like blood clots and encourages circulation.
Common Post-Surgery Symptoms
It’s normal to experience a range of physical symptoms after gastric sleeve surgery. Being aware of what’s to be expected can help you stay calm throughout recovery.
- Pain and Soreness: Mild to moderate pain around the incision sites is normal. Your care team will provide prescription or over-the-counter pain relief to manage this.
- Nausea and Vomiting: These can occur, especially after your first sips of clear liquids. They usually subside quickly as your body adjusts. Staying hydrated and following your surgeon’s dietary guidelines can help improve this.
- Fatigue: Feeling tired is common in the early days of recovery. Your body is healing, and rest is essential to support that process.
- Gas or Bloating: The gas used during laparoscopic surgery can cause discomfort in your abdomen or shoulders. Walking and light movement help to alleviate this.
While these symptoms are expected, there are signs that demand immediate medical attention:
- High fever or chills
- Severe or worsening pain
- Shortness of breath
- Unusual swelling, redness, or drainage at your incision site
If you notice any of these, contact your surgeon or visit the emergency room without delay. Your safety and recovery go hand in hand.
Mental and Emotional Adjustments
The physical adjustments following surgery can be an emotional rollercoaster in the weeks and months after your procedure. It’s not uncommon to feel excited about your progress but also a bit anxious about the lifestyle changes ahead.
Initially, you may go through waves of emotion as your body recovers and adjusts to rapid weight loss. Hormonal changes, combined with the physical stress of surgery, can impact your mood. This isn’t a sign of failure—it’s part of the process.
Some patients feel a sense of loss or grief surrounding their old relationship with food. Meals aren’t just fuel; they’re tied to memories, celebrations, and social gatherings. Adapting to a smaller stomach may mean finding new ways to enjoy those moments, and that can take time.
Lean on your support system, whether it’s family, friends, or a therapist experienced in weight-loss surgery. Share your feelings and set realistic goals. Remember, this is a journey, not an overnight transformation. Stay patient with yourself and focus on the progress you’re making, both physically and emotionally.
Embrace this opportunity to not only rebuild your body but also create a healthier mindset and lifestyle. If you find yourself struggling, connect with others who’ve walked the same path—they can offer valuable insight and encouragement.
Dietary Guidelines During Recovery
Your recovery diet after gastric sleeve surgery isn’t just a temporary routine—it’s the cornerstone of your healing process. This staged approach allows your body to recover while gradually adapting to the reduced size of your stomach. Each phase comes with its own set of rules and focuses on gentle progression, ensuring you get the nutrients you need without straining your digestive system.
Let’s break it down into four key phases of your post-surgery diet.

Phase 1: Clear Liquids
The first week after surgery revolves around clear liquids, and for good reason. Your stomach is in a fragile state, healing from the procedure and adjusting to its smaller size. Clear liquids provide hydration, help with nutrient absorption, and are easy on your digestive system.
So, what can you consume? Here’s a quick list:
- Water (sip slowly throughout the day, aiming for at least 48–64 ounces daily).
- Broths (low-sodium chicken, beef, or vegetable broth are best).
- Sugar-free flavoured drinks (like diluted squash or electrolyte beverages).
- Herbal teas (decaffeinated options like chamomile are soothing).
- Gelatine or ice lollies (make sure they’re sugar-free).
Avoid anything with sugar, caffeine, or carbonation—these can irritate your stomach or cause discomfort. Sip everything slowly; gulping can lead to nausea or pain. If you find it difficult to get enough liquids in at first, don’t worry. Do your best, and keep aiming for gradual improvement daily.
Phase 2: Full Liquids
Once your surgeon gives the green light, typically around week two, you’ll move on to full liquids. This stage continues to prioritise hydration and gentle digestion but introduces liquids with more nutrition and substance.
Full liquids include everything from Phase 1, plus heartier options like:
- Protein shakes (low-sugar, high-protein options are ideal).
- Smooth soups (blended soups made from vegetables or chicken with no chunks).
- Milk (skimmed or semi-skimmed, depending on your dietary needs).
- Greek yoghurt (plain, unsweetened, or flavoured with no added sugars).
- Oat or rice milk (plain and unsweetened).
Protein becomes a key focus during this phase. Aim for at least 20–30 grams of protein a day to support muscle repair and healing. Avoid fibrous or chunky ingredients in soups, and always strain them to ensure smooth consistency. Drink or eat slowly—listening to your body is critical to avoid overwhelming your stomach.
Phase 3: Pureed Foods
Around weeks three and four, you’ll enter the pureed phase. Think of baby food textures here: soft, smooth, and easy-to-digest options. Your stomach is still healing, so small portions are a must.
This is your first introduction to more nutrient-dense solid foods. Ideal choices include:
- Mashed or blended fruits (like banana or applesauce, unsweetened).
- Cooked, blended vegetables (potatoes, carrots, or spinach without skins or fibres).
- Lean proteins (like pureed chicken, turkey, or fish).
- Scrambled eggs (well-cooked and mashed).
- Cottage cheese or ricotta cheese.
Stick to three small meals a day and avoid snacking. Portion control matters—start with just a couple of bites at a time and slowly increase if tolerated. The goal is to eat slowly, chew thoroughly, and listen to how your body reacts.
Foods to avoid include anything spicy, acidic, or textured, as these can irritate your stomach lining and slow healing. Keep sipping water between meals to stay hydrated, but wait at least 30 minutes after eating to drink.
Phase 4: Solid Foods
Finally, solid foods are back on the table around week five or six, depending on your surgeon’s advice. This phase is all about slowly reintroducing texture while continuing to focus on portion control and proper nutrition.
Start with soft, easy-to-chew foods like:
- Steamed vegetables (choose tender, non-fibrous options).
- Lean meats (grilled chicken or fish, finely chopped).
- Whole fruit (peeled and diced, avoiding anything too tough or fibrous).
- Whole grains (oatmeal or quinoa, fully cooked and soft).
It’s crucial not to rush. Cut your food into small pieces, and eat mindfully. Your stomach can only handle a small amount at a time, often about 4–6 ounces per meal. Overeating can lead to discomfort, nausea, or even vomiting.
Stay away from hard-to-digest foods, such as:
- Tough cuts of meat.
- Foods high in fat (fried or greasy options).
- Crispy snacks like chips.
- Processed sugar (cakes, sweets, etc.).
Portion control is your best friend on this journey. Measuring your food can help you stay on track and prevent overloading your stomach. Continue to prioritise hydration, but as always, avoid drinking with meals to allow your stomach to process food more efficiently.
By following these phases closely, you’re setting yourself up for a smoother recovery and a healthier future. Each stage builds on the previous one, helping your body adjust with minimal stress. Remember, patience is key—every small step leads to significant progress.
Physical Activity and Recovery
Moving your body after gastric sleeve surgery is an essential part of your recovery. While rest is crucial in the early days, incorporating physical activity into your routine helps prevent complications and supports healing. However, not all exercises are appropriate right away, and you’ll need to ease into it with care. Here’s a guide to when and how to move safely during recovery.

When to Start Moving
In most cases, your surgeon will encourage you to start moving within the first 24 hours after surgery. This doesn’t mean jumping into a workout—it’s as simple as sitting up in bed or taking a short walk around the hospital room.
By the time you’re home, light activity like leisurely walking becomes a daily priority. Walking promotes blood flow, reduces swelling, and lowers the risk of serious complications like blood clots.
Here’s a rough timeline for getting started safely:
- Day of Surgery: You may sit up or stand with assistance, depending on how you feel.
- Days 2–3: Take short, slow walks inside your home—no more than five minutes at a time.
- End of Week 1: Gradually increase your walking to about 10–15 minutes as tolerated, once or twice a day.
It’s perfectly normal to feel tired or slightly sore, but stop immediately if you feel dizzy, short of breath, or experience abdominal pain.
Exercise Guidelines by Weeks
Your physical activity will progress as your body heals. Following a structured timeline ensures you’re not overdoing it too soon while still reaping the benefits of movement.
Week 1–2: Focus on Gentle Movement
- Stick to light walking only. A stroll around the house or a gentle walk outside when you feel ready.
- Avoid all forms of weightlifting, bending, or twisting motions.
- Take rest breaks if needed; the goal is to keep circulation moving, not to exhaust yourself.
Week 3–4: Gradual Strength Building
- Increase walking duration gradually, aiming for at least 20–30 minutes daily if comfortable.
- Introduce very light stretching, focusing on easing muscle tension rather than forcing flexibility.
- Continue avoiding intense exercises like running or aerobics—your body isn’t ready just yet.
Week 5–6: Low-Impact Activity
- Consider adding low-impact options like light cycling or swimming (once cleared by your surgeon).
- Engage in basic bodyweight exercises like heel raises or wall push-ups, but avoid core-focused workouts.
- Start building a sustainable habit of daily activity without overloading your energy levels.
Week 7+: Begin Customised Routines
At this stage, many patients are ready for more challenging activities, depending on individual recovery. You might include strength training with light weights or engage in yoga or pilates to build stability and balance. Always consult your surgeon or healthcare provider before progressing to higher-intensity routines.
Avoiding Strain
While it’s tempting to speed up recovery by pushing yourself, this can do more harm than good. Strenuous activities can stress your healing body, delay recovery, or even lead to complications. Knowing what to avoid is just as important as knowing what to do.
Here are a few activities that should be off-limits in the early stages:
- Lifting Heavy Objects: Avoid lifting anything over 4–5 kg for at least six weeks. Even household tasks like grocery shopping or lifting a laundry basket should be approached cautiously.
- Abdominal Exercises: Skip sit-ups, planks, or any activity that works your core directly until your surgeon clears you. Overworking these muscles early on can strain your incision site.
- High-Impact Workouts: Running, jumping, or any activity involving sudden, jarring movements is not suitable during your recovery phase.
- Twisting Motions: Movements like yoga twists or reaching behind you can stretch healing tissues, potentially causing pain or damage.
Above all, listen to your body. If something doesn’t feel right or causes discomfort, stop. Recovery isn’t about how quickly you can resume your normal routine—it’s about creating a foundation of healthy habits that will support your new lifestyle.
Tips for Long-Term Success
Once you’ve made it through the initial stages of gastric sleeve recovery after surgery, the focus shifts to long-term success. Achieving your goals isn’t just about losing weight—it’s about building sustainable habits, staying motivated, and understanding the tools and support available to help you thrive. This section provides practical tips on how to ensure your progress lasts well beyond the recovery period.
Building Healthy Eating Habits
Eating after gastric sleeve surgery involves more than smaller portions—it’s an entirely new relationship with food. You need to prioritise thoughtful choices while ensuring you’re meeting your nutritional needs.
Here are some tips for creating lasting healthy eating habits:
- Plan Your Meals: Meal planning keeps you on track and helps you avoid impulsive food choices. Prepping meals ahead of time ensures you’ll always have balanced options, reducing the temptation to grab unhealthy snacks.
- Focus on Protein First: Your stomach’s new size means you can only eat small amounts, so focus on high-protein foods like lean meats, eggs, or beans. Protein is essential for healing and muscle maintenance.
- Eat Slowly and Mindfully: Chew every bite thoroughly and take your time. Eating too quickly can lead to discomfort or overeating. Pay attention to your body’s signals—when you’re full, stop eating.
- Avoid Liquid Calories: Sugary drinks or high-calorie beverages can add up quickly and derail your progress. Stick to water, herbal teas, or other low-calorie options.
- Practice Portion Control: Invest in smaller plates or bowls to help you visualise appropriate servings. Measuring your portions can also help you stay consistent.
Making these behaviours part of your routine takes patience, but consistency is key. Think of it like learning a new skill—it becomes second nature over time.
Setting Realistic Goals
Setting achievable goals is one of the most important ways to maintain long-term success and avoid frustration. It’s tempting to aim for monumental changes right away, but small, steady progress often leads to better outcomes.
- Divide Your Goals into Stages: Instead of focusing on one big number, break your weight-loss goal into smaller milestones. Celebrating these achievements keeps you motivated along the way.
- Prioritise Health Over Numbers: While the scale can be a helpful tool, don’t get overly fixated on it. Success isn’t only about weight—it’s about feeling healthier, having more energy, or reaching fitness benchmarks.
- Be Prepared for Plateaus: Weight loss isn’t linear, and it’s normal to hit a plateau. When this happens, revisit your habits and look for small adjustments that can kick-start progress.
- Track Progress in Different Ways: Don’t limit progress tracking to weight alone. Use other measures, like how your clothes fit, energy levels, or fitness achievements, to gauge success.
- Be Patient with Yourself: Changes don’t happen overnight. Focus on developing a lifestyle you can maintain for years, not just months.
Setting realistic, measurable goals gives you a clear roadmap to follow, making success feel both achievable and rewarding.
Support Systems and Resources
No one succeeds entirely on their own, especially when it comes to significant life changes like those following gastric sleeve surgery. A strong network of support can make all the difference in staying accountable, motivated, and focused.
Who should be in your corner?
- Friends and Family: Let them know what you’re going through and how they can support you. Whether it’s helping you stay active, cooking healthy meals together, or simply offering encouragement, their role is vital.
- Professional Support: Regular follow-ups with your surgeon or dietitian ensure you’re on the right path. They can provide guidance tailored to your progress, troubleshoot any issues, and keep you motivated.
- Support Groups: Joining a weight-loss surgery group, either in-person or online, connects you with others who understand your journey. These communities often share practical tips, advice, and emotional support for challenges you may face.
- Mental Health Resources: Therapy can be particularly helpful in addressing the emotional adjustments after surgery. If you’re struggling with body image, food anxiety, or other concerns, a mental health professional can provide strategies to cope.
Remember, reaching out for support isn’t a sign of weakness—it’s a way to strengthen your own resolve. You’re much more likely to succeed when you surround yourself with positive influences who encourage and empower you.
Making long-term changes can feel challenging, but with the right habits, realistic goals, and an active support system, you’ll be well-positioned to maintain your progress and lead a healthier, happier life.
Recognising and Addressing Complications
Complications after gastric sleeve surgery are rare but can happen. Staying aware of potential red flags and knowing when to seek help is essential for a smooth recovery. Being proactive about your health can prevent minor issues from escalating into something serious. Let’s explore the key aspects of recognising and addressing complications.
Signs of Post-Surgical Complications
While mild discomfort, fatigue, and soreness are a normal part of healing, some symptoms might signal a more significant problem. Pay attention to your body, and don’t ignore symptoms that feel out of the ordinary.
Here are some warning signs to watch for:
- Severe Pain: If pain becomes sharp or doesn’t improve over time, it could indicate something isn’t healing correctly.
- High Fever or Chills: A fever above 38°C may be a sign of infection.
- Redness or Swelling Around Your Incision: This could point to an infection, especially if the area feels warm to the touch or starts to drain pus.
- Persistent Vomiting or Nausea: Occasional nausea is normal, but constant vomiting can lead to dehydration and should be investigated.
- Unusual Bleeding: Spotting is common, but if you notice significant bleeding or blood in your stool, it’s time to act.
- Difficulty Breathing: Shortness of breath or chest discomfort might point to a blood clot or other serious issues.
- Unexplained Weakness: Feeling faint, overly fatigued, or lightheaded could indicate dehydration, nutrient deficiencies, or another underlying issue.
Trust your instincts. If something feels off or if symptoms worsen, it’s better to get it checked out sooner rather than later.
When to Contact Your Surgeon
So, when should you pick up the phone and call your surgeon? Here’s a straightforward guideline to follow.
Call your surgeon immediately if you experience:
- Intense, Unrelenting Pain: Especially in your abdomen or shoulder area.
- Signs of Infection: Fever, chills, or drainage from your incision site.
- Excessive Bleeding: Any bleeding that seems out of the ordinary or won’t stop.
- Difficulty Swallowing: If liquids or soft foods aren’t going down easily.
- Breathing Issues: Sudden shortness of breath or chest pain requires urgent attention.
- Rapid Heartbeat: A racing heart unrelated to physical activity should be assessed.
Don’t downplay your symptoms to avoid a “wasted” trip—your surgeon and medical team are there to help. When in doubt, it’s always safer to over-communicate than ignore potential issues.
Maintaining Regular Follow-Ups
Routine follow-up appointments are a cornerstone of your recovery process. These check-ups aren’t just a box to tick—they allow your healthcare team to monitor how your body is healing, spot complications early, and guide you through any challenges.
Here’s why regular visits matter:
- Progress Monitoring: Your doctor will check how you’re healing, track your weight loss, and ensure you’re meeting your nutritional needs.
- Adjusting Your Care Plan: If an issue arises—whether it’s slow healing, nutrient deficiencies, or dietary struggles—your care team can make adjustments to keep you on track.
- Long-Term Health: Follow-ups help assess any long-term effects of the surgery, such as vitamin deficiencies or ongoing weight-loss progress.
Generally, your surgeon may schedule visits or online meetings:
- Within the first week after surgery.
- At the end of the first month.
- At the 3-, 6-, and 12-month marks.
- Annually thereafter to check your long-term health.
If your appointments feel overwhelming or rushed, come prepared. Write down any questions or concerns ahead of time so you make the most of your visit.
Last Words from the More Clinics
The gastric sleeve recovery journey is a transformative process that requires dedication and commitment. By understanding what to expect and following the short and long-term recovery tips, you can achieve a successful and fulfilling recovery after gastric sleeve surgery. Remember, your healthcare provider is your best resource throughout this journey, providing guidance and support to ensure a healthier and happier you.
At The More Clinics, our experienced medical team is committed to helping you achieve your weight loss goals through gastric sleeve surgery and comprehensive aftercare. Contact us today to learn more about our bariatric surgery options and start your journey to a healthier life today.
GET A FREE CONSULTATION!
Let’s Start Planning Your Treatment %100 Guarantee Results.
FAQs Gastric Sleeve Surgery Recovery
Though it varies between individuals, generally, patients take about 2 to 4 weeks to fully recover from gastric sleeve surgery. However, the journey towards adapting to lifestyle changes and a new diet plan can continue for several months following the procedure.
Yes, you can return to work after gastric sleeve surgery, typically within 1-3 weeks, depending on the nature of your job. If your work involves strenuous activity, you may need to wait longer and should consult your healthcare provider.
You can begin with light physical activities such as walking shortly after surgery. However, you should avoid rigorous exercise until approximately 4 weeks post-op. Always consult your healthcare provider before starting any new exercise regimen.
It typically takes 4-6 weeks for your stomach to heal after sleeve gastrectomy.
You should wait at least 2 weeks before driving, and make sure you are not taking any pain medications that could impair your driving skills. Check with your healthcare provider for further guidance.
Yes, mild to moderate diarrhea is common in the early days after gastric sleeve surgery. However, if the symptoms persist or worsen, consult your healthcare provider promptly.
Yes, a metallic taste is common post-surgery and usually disappears within a few weeks. Consult your healthcare provider if this symptom persists.
It is best to avoid alcohol for the first three months following gastric sleeve surgery, as it could interfere with your recovery process and nutritional absorption. After this period, you may be able to safely consume occasional amounts of light alcoholic drinks in moderation. Consult your healthcare provider for further guidance.
es, there are several other bariatric surgery options available such as Laparoscopic Roux-en-Y Gastric Bypass, Biliopancreatic Diversion with Duodenal Switch (BPD/DS), and Vertical Sleeve Gastrectomy. For Comparison of Gastric Sleeve and Gastric By Pass.
SOURCES:
“Postoperative Care and Functional Recovery After Laparoscopic Sleeve Gastrectomy vs. Laparoscopic Roux-en-Y Gastric Bypass Among Patients Under ERAS Protocol”
“Long-term complications and side effects of bariatric surgery: a
systematic review”
“The advantages and disadvantages of sleeve gastrectomy; clinical laboratory
to bedside review”
“The effects of bariatric surgical procedures on the improvement of metabolic syndrome in morbidly obese patients: Comparison of laparoscopic sleeve gastrectomy versus laparoscopic Roux-en-Y gastric bypass”
HOW THE MORE CLINICS KEEP THE CONTENT UP TO DATE:
Our dedicated medical and editorial teams work tirelessly to stay informed about the ever-evolving world of health news. By rigorously tracking the latest research, clinical guidelines, and significant developments across various medical fields, they ensure that our content remains accurate, relevant, and up-to-date. This includes reviewing peer-reviewed studies, consulting with healthcare professionals, and monitoring advancements in medical technology. Their meticulous efforts and attention to detail allow us to provide you with trustworthy, reliable information that you can depend on to make informed decisions about your health and well-being.
However, we still insist on getting a healthcare professional’s opinion before you make any decision about your health. Consulting with a qualified expert ensures that the choices you make are informed, safe, and tailored to your individual needs.
Last Uptaded at: February 28, 2025
Medically Reviewed by: NAMIK YILMAZ, MD, BARIATRIC SURGEON